Parkinson’s disease, a neurodegenerative disorder characterized by tremors, stiffness, and slow movements, can significantly impact an individual’s quality of life. Physical therapy plays a vital role in managing the symptoms of Parkinson’s and improving functional abilities. Check how it can help below:
It’s well-known that exercise of all kinds is beneficial for patients with Parkinson’s disease. But physical therapy, in particular, is key. Why? A professional can guide you through the right moves to increase mobility, strength and balance, and help you remain independent, says Denise Padilla-Davidson, a Johns Hopkins physical therapist who works with patients who have Parkinson’s. Here are things a therapist may work on:
Note: Please discuss any exercise program with your physician/neurologist and get a referral to a physical therapist or trainer with expertise in Parkinson’s disease before starting any specific program.
Amplitude Training
A specific form of physical therapy for Parkinson’s disease is called LSVT BIG training. (LSVT is Lee Silverman Voice Treatment. LSVT LOUD is therapy to amplify the voice.) “It’s meant to help patients with Parkinson’s increase what we call ‘amplitude of movement,’” says Padilla-Davidson. In LSVT BIG, you make overexaggerated physical movements, like high steps and arm swings. It’s a way to retrain the muscles and slow down the progression of hypokinesia, the increasingly smaller, more shuffling movements that happen with Parkinson’s. Ask your doctor or physical therapist about LSVT BIG.
Reciprocal Patterns
Reciprocal movements are side-to-side and left-to-right patterns, such as swinging your arms while taking steps as you walk. Parkinson’s disease may affect these patterns. Your therapist may help you reinforce reciprocal patterns by the use of a recumbent bicycle (a stationary bike in which you sit in a reclined position) or elliptical machine (in which you use your arms and legs). On your own, says Padilla-Davidson, “Practice walking, keeping in mind the swinging of your arms. It may help to chant or sing to keep the rhythm.” Dance classes and tai chi are also useful.
Balance Work
Normal balance, explains Padilla-Davidson, is an interplay among what you see (visual feedback), your inner ear (which helps you orient yourself) and how your feet sense the ground beneath them. Parkinson’s disease can affect this balance system, making your gait (how you walk) unstable, which in turn may make you fearful to be in public or crowded spaces. Gait training (practice walking) can help. Exercises that aim to improve balance should be guided by a physical therapist, who can work with you to understand any issues with balance and teach you ways to compensate.
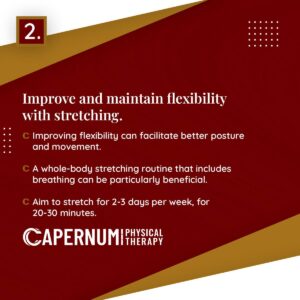
Stretching and Flexibility
It’s common for patients with Parkinson’s disease to develop tight hip flexor, hamstring and calf muscles. To counteract that stiffness, it’s best to stretch at frequent intervals throughout the day, rather than just once, says Padilla-Davidson. Ask a qualified trainer or therapist who specializes in Parkinson’s to show you how.
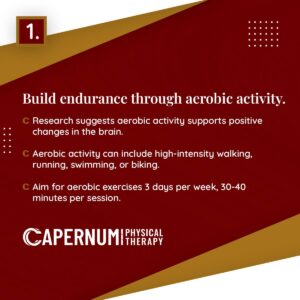
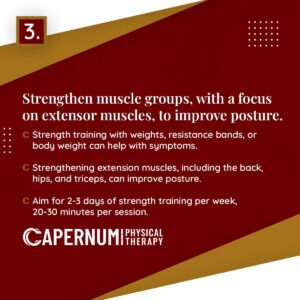
Strength Training
Muscles naturally weaken with age, so strength training is important for everyone. But research suggests that muscle weakness is a bigger problem for patients with Parkinson’s disease, says Padilla-Davidson. Depending on what stage of the disease you are in, a therapist might have you do resistance exercises with light dumbbells or a resistance band (a kind of thick rubber band). Pool-based classes, using the water’s resistance to strengthen muscles, can also be a good fit, she says.
Take control of your Parkinson’s journey. Let our physical therapy specialists enhance your strength, balance, and coordination with a personalized treatment plan. Call us today at 201.308.3884 or join our Instagram community here.
Reference: [https://www.hopkinsmedicine.org/health/conditions-and-diseases/physical-therapy-for-parkinsons-disease]